This article is part of our feature The Politics of Health Equity in Europe.
Mircea,[1] a former miner in his fifties, spent the last four years of his life succumbing to Extensively Drug Resistant Tuberculosis (XDR-TB)[2] at the Pines Tuberculosis Sanatorium, which is located high on a mountain. After seven years with this otherwise curable illness, his family wanted little to do with him. He was one of the many patients who doctors in Romania refer to as “social cases”[3] [4]According to Dr. Ionescu at the Pines, patients like Mircea are “repeat clients” with “no chance of escape.” They are people with overlapping social and economic difficulties, such as poverty, homelessness, alcohol use, lack of family support, as well as the social stigma that comes with having TB in Romania.
In November 2015, the United Nations Human Rights Council Special Rapporteur on extreme poverty and human rights, Philip Alston, stated that “[m]any officials are in a state of denial about both the extent of poverty in the country and of the systemic and deep-rooted discrimination against the extremely poor, especially the Roma.”[5]
Romania is one of the poorest countries in the European Union (EU), with 40 percent of the population living in or at risk of poverty.
[6] While politicians and community leaders may have denied Romania’s poverty, Alston, the patients, and the medical staff I worked with did not; in fact, their focus on it may have distracted attention from other problems.
This post is less about poverty at the individual, community, or even health-system level, and more about the things we miss when we fail to investigate contributing factors beyond those most visible. I focus here on the “unknown unknowns,” [7] which are present in the background, yet unable to be discovered because they may be unknown not just to the researcher, but to their research participants as well.
My research into the issue of TB in Romania has so far included five years of fieldwork between 2006 and 2014, and included six months living at one of Romania’s largest TB sanatoria. Yet, it was only toward the end of my research that I discovered these unknown unknowns. The initial focus of my research was what I described as a medicalization of social welfare, which was occurring at institutions such as TB sanatoria, where doctors extended the stays of patients who had nowhere else to go. Romania’s health and social welfare systems have been largely neglected since the early 1980s. Doctors often must choose between providing a poor, elderly, or homeless person temporary protection in a medical unit, or rejecting them knowing that they will be living on the streets.
When I asked patients, medical staff, workers for non-governmental organizations, and others why so many people were dying of drug-resistant TB in Romania, they usually responded by telling me about poverty. Some blamed the patients, stating that they were irresponsible, alcoholic, Roma (gypsy—which in Romania is shorthand for everything negative), or poorly educated. Others avoided blaming the victims. Instead, they told me about structural issues such as unemployment, de-industrialization, and lack of support for poor families.
These latter explanations are all true. But was it really just poverty that was keeping drug-resistant TB patients from being cured? During most of my fieldwork, Romania had treatment success rates for MDR-TB and XDR-TB of between 16 percent and 20 percent.[8] These were among the lowest recorded anywhere in the world. Yet, Romania is an upper-middle income country in the EU and wealthier than countries that were curing patients at rates up to 75 percent.[9]
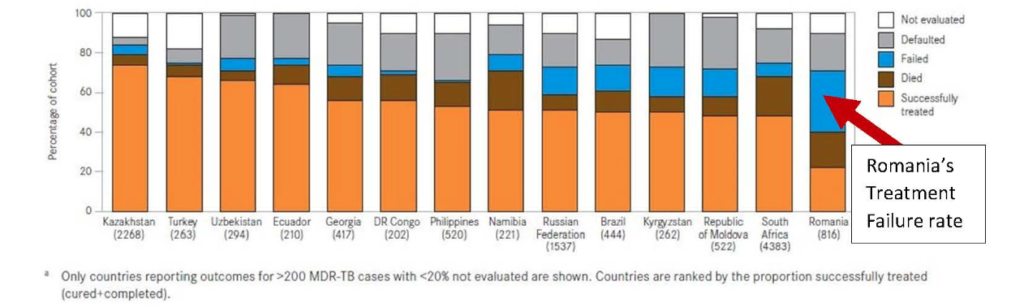
Not only did Romania have one of the lowest rates of MDR-TB and XDR-TB treatment success in the world, it also recorded a rate of treatment failure of about 40 percent. Yet, the chart above does not simply point to poverty as the driver of TB deaths; nor are these deaths merely explained by issues such as alcohol use or running away from the hospital. In contradiction with these explanations, patients were treated for the full duration (two to three years) under a doctor’s supervision, yet they were never cured.
High rates of MDR-TB and XDR-TB treatment failure in Romania are best explained by weak treatment regimens, drug shortages, and drug stock-outs. These problems have been well documented since at least 2009 and continued to complicate treatment through 2014.[10] [11] [12] [13] These drug shortages were happening throughout my fieldwork, and patients were dying in large numbers. Most doctors were not denying the stock-outs. Rather, they told me that poverty was the main problem.
The truth is that patients such as Mircea and most of those with MDR-TB and XDR-TB whom I came to know at the Pines and across Romania were indeed poor. Nevertheless, with the exception of a small group treated at two special centers supported by the Global Fund, most of them were not getting adequate treatment. Drugs required for treatment were missing for sometimes months at a time. Moreover, weaker, cheaper drugs were being used instead of those conforming to international standards.[14] One of the most important gaps was the general absence of injectable second-line antibiotics. I rarely saw these outside of the two internationally funded centers, even though they are considered to be a required part of MDR-TB treatment.[15]
Some medicines used throughout the world for treating MDR-TB and XDR-TB are still unavailable in Romania. I did not see these gaps until I learned the technical aspects of TB diagnosis, treatment, and later—and most importantly—the local and international regulations and procedures governing drug procurement.
In fact, some of the issues related to procurement were not even known to the doctors and other experts who were responsible for procuring these drugs.
Changes in local law and unfamiliar EU regulations complicate matters. Romania is in the awkward position of not being able to benefit from some of the donated medicines and discounted pricing that non-EU countries in the region, such as neighboring Moldova, enjoy. Because the initial problem was always a lack of funds, no one realized that beyond money, there were regulatory issues that would prevent patients from getting the treatment they needed, even after funding became available.
Today, when the social aspects of any disease are discussed by policymakers, civil society members, and medical staff, the focus is overwhelmingly on individual and community-level issues such as poverty, alcohol, and drug use. This is especially true with TB. Yet, we rarely think of poverty in terms of health systems. As Alston mentions in his report: “I was often told that poverty is a choice. It is indeed, but the choice is too often made by government policies rather than by those living in poverty.”[16] An example of this are the policies ensuring that Romania’s Ministry of Health receives one of the lowest rates of funding (as a percentage of gross domestic product) in the entire European region.
Early thinking about social diseases, such as Rene and Jean Dubos’s (1952) and Randall Packard’s (1989), pointed to the effects of industrialization and capitalist exploitation of labor as the best explanations for TB. Others, such as Paul Farmer, have called for a broader view of social diseases that looks more closely at the effects of structural violence (2001). More recently, Erin Koch has stressed the importance of considering within the social the effects of modern technological innovations such as diagnostics and “the rise of bacteriology and bacteria as social actors” (2013, 13).
I would add to this that the “social” in social diseases must also include a serious examination of local, national, and regional (particularly the EU) laws and regulations that govern intellectual property; the import and export of medicines and diagnostic technologies; the systems through which these technological innovations are procured, stored, and distributed; local, national, and international funding mechanisms; and finally, how local, national, and international politics shapes the health systems that patients, medical staff, and social scientists encounter. These harder-to-see social factors may be the “unknown unknowns” in one’s field site. As I discovered, they may not even be fully understood by local and national experts. For this reason,
a healthy dose of self-doubt and an appreciation for the technical, legal, and bureaucratic aspects of our field sites are important.
Mircea told me in 2010 that he felt abandoned by his family and government, but that he hoped he would get better. His reason to live was his 4-year-old granddaughter whom he had only seen in pictures. It was only after the deaths of most of my research participants that I realized that, despite their hopes for the future, they were not getting better. It was not poverty that was killing Mircea (although poverty complicated matters and perhaps prevented him from demanding better care). The medications he and the majority of Romanians with MDR-TB and XDR-TB received between 2008 and 2014 were not adequate to cure them. Therefore, while poverty contributed to their illness, no one, rich or poor, can be cured with weak and incomplete treatment.
My intention is not to minimize the issue of poverty in understanding Romania’s TB situation. TB is strongly associated with poverty. It greatly increases one’s risk of developing TB, exacerbates it, and makes treatment more difficult. However, it is necessary to view poverty in conjunction with factors, which might seem overly specialized or technical if one is to discover complete explanations for the phenomena encountered during fieldwork.
This may be challenging, especially in the context of ever-shrinking fieldwork duration. Nevertheless, if other, more technical issues are not considered, we risk at best presenting well-meaning, though incomplete, pictures, and at worst, producing what Farmer has called “immodest claims of causality,” which do our research participants a disservice and, ultimately, may do more harm than good by directing local and international attention away from the true causes of their deaths (2001).
Jonathan Stillo is an Anthropology candidate at the CUNY Graduate Center, and an Adjunct Lecturer at Hunter College.
Photo: Gyspy Brothers 3, Jake Stimpson | Flickr
References:
[1] All proper names are pseudonyms.
[2] There are three types of TB: Drug susceptible, for which treatment lasts six months and includes four antibiotics; Multi Drug Resistant (MDR-TB), which is resistant to the two most powerful TB drugs and generally takes 18–24 months to treat; and Extensively Drug Resistant (XDR-TB) which is MDR-TB that is also resistant to two additional classes of drugs and can take three years to cure.
[3] Friedman, Jack. 2009. “The ‘Social Case’: Illness, Psychiatry, and Deinstitutionalization in Post-Socialist Romania.” Medical Anthropology Quarterly 23 (4): 375-96.
[4] Stillo, Jonathan. 2012. “‘All My Problems Started with Tuberculosis’: An Ethnographic Analysis of Treatment Failure in Romania.” IREX Scholar Research Brief. February.
[5] Alston, Philip. 2015. “End-of-Mission Statement on Romania.” November 11. http://www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=16737&LangID=E (March 11, 2016).
[6] Alston, Philip. 2015. “End-of-Mission Statement on Romania.” November 11. http://www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=16737&LangID=E (March 11, 2016).
[7] “Unknown unknowns” was popularized by former United States (US) Secretary of Defense Donald Rumsfeld. In his memoir, he credits the phrase to US National Aeronautics and Space Administration (NASA) Administrator William Graham.
[8] World Health Organization and the European Center for Disease Control and Prevention. 2015. “Review of the National Tuberculosis Programme in Romania, 10–21 March 2014.” http://www.euro.who.int/__data/assets/pdf_file/0007/269269/Review-of-the-national-tuberculosis-programme-in-Romania.pdf?ua=1 (March 11, 2016).
[9] World Health Organization. 2011. “Report: Global Tuberculosis Control.” http://apps.who.int /iris/bitstream/10665/44728/1/9789241564380_eng.pdf (March 11, 2016).
[10] World Health Organization and the European Center for Disease Control and Prevention. 2009. “Review of the National Tuberculosis Programme in Romania.” Copenhagen: WHO.
[11] World Health Organization and the European Center for Disease Control and Prevention. 2015. “Review of the National Tuberculosis Programme in Romania, 10–21 March 2014.” http://www.euro.who.int/__data/assets/pdf_file/0007/269269/Review-of-the-national-tuberculosis-programme-in-Romania.pdf?ua=1 (March 11, 2016).
[12] Yedilbayev, Askar 2012, “GLC/Europe Mission for Monitoring of the Implementation of the National M/XDR-TB Response Plan in Romania.” April 23-28. http://stop-tb.ro/wp-content/uploads/2014/10/GLC_Report_2012_eng.pdf (March 11, 2016).
[13] Stillo, Jonathan. 2012. “‘All My Problems Started with Tuberculosis’: An Ethnographic Analysis of Treatment Failure in Romania.” IREX Scholar Research Brief. February.
[14] Specifically, ciprofloxacin remained in wide use in Romania through at least 2013, despite a global recommendation from WHO in 2008 to cease using it for TB because of its weak action (WHO 2008; Yedilbayev 2012).
[15] World Health Organization. 2014. “Companion Handbook to the WHO Guidelines for the Programmatic Management of Drug-Resistant Tuberculosis.” http://apps.who.int/iris /bitstream/10665/130918/1/9789241548809_eng.pdf?ua=1&ua=1 (March 11, 2016).
[16] Alston, Philip. 2015. “End-of-Mission Statement on Romania.” November 11. http://www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=16737&LangID=E (March 11, 2016).